The Open Data Institute (ODI) has today published findings from a research study by Frontier Economics, which looks at social prescribing across England. We have also published a digital tool from Mime Consulting, which looks at social prescribing demand indicators across England.
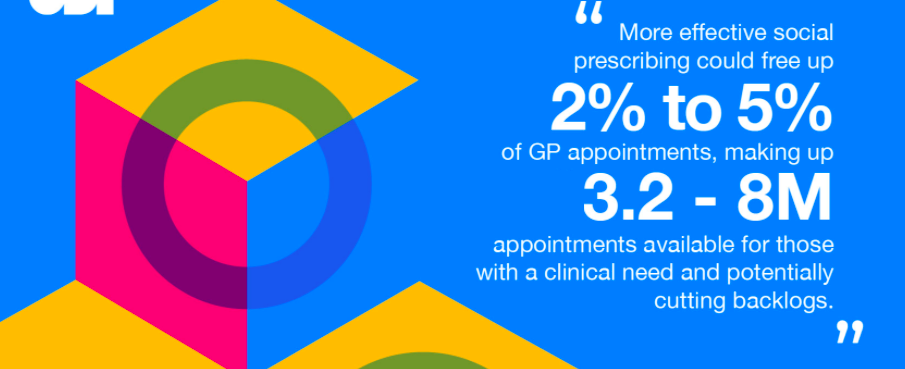
More effective social prescribing could free up 2% to 5% of GP appointments, making up 3.2-to 8 million appointments available for those with a clinical need, and potentially cutting backlogs. But data infrastructure is currently a weak link in the social prescription model, which means that resources may not be directed appropriately.
Social prescribing is working to combat loneliness, mental health and welfare issues while helping to improve physical health. New digital data tool allows NHS and local authorities to examine social and health issues that may see patients present for a social prescription.
The role of data in unlocking the potential of social prescribing highlights the importance of data to those working in social prescribing. GPs, link workers, charities and other health and wellbeing practitioners could more effectively target issues such as mental health and improve provision of non-clinical interventions, from physical activity to assistance with social or welfare problems with improved data availability.
"This new report shows that social prescribing can unlock health and societal benefits more efficiently if certain enablers are in place. One such enabler is the need for data infrastructure, by which we mean the standards and stewardship to enable collection and sharing of appropriate information. If GP appointments can be reduced in the way that the report indicates then this is a clear case of how efficient collation and sharing of data can have sizeable benefits for the NHS" – ODI Managing Director, Louise Burke
The report highlights how social prescribing, if it were to reach its full potential, could lead to improved health, redirected demand for NHS services, improved community cohesion and greater economic productivity.
"If GPs could redirect even 1% of our current caseload to social prescribers, we not only get these people to the right place first time, we also create more capacity to deal with some of the unmet demand and huge backlog facing the NHS as a result of covid. If a 4% reduction could be possible as this report suggests, that means a real difference to patients in terms of better health and wellbeing outcomes, and more people overall seeing a benefit.” – Dr Ben Molyneux GP, clinical lead for social prescribing and personalised care in North East London
The report finds that there are a number of barriers to social prescribing reaching its full potential, amongst them the lack of available data, and solid data infrastructure. Data infrastructure is information such as statistics, maps and real-time service-use data that could help social prescribers and the providers of services to make decisions, build services and gain insight.